
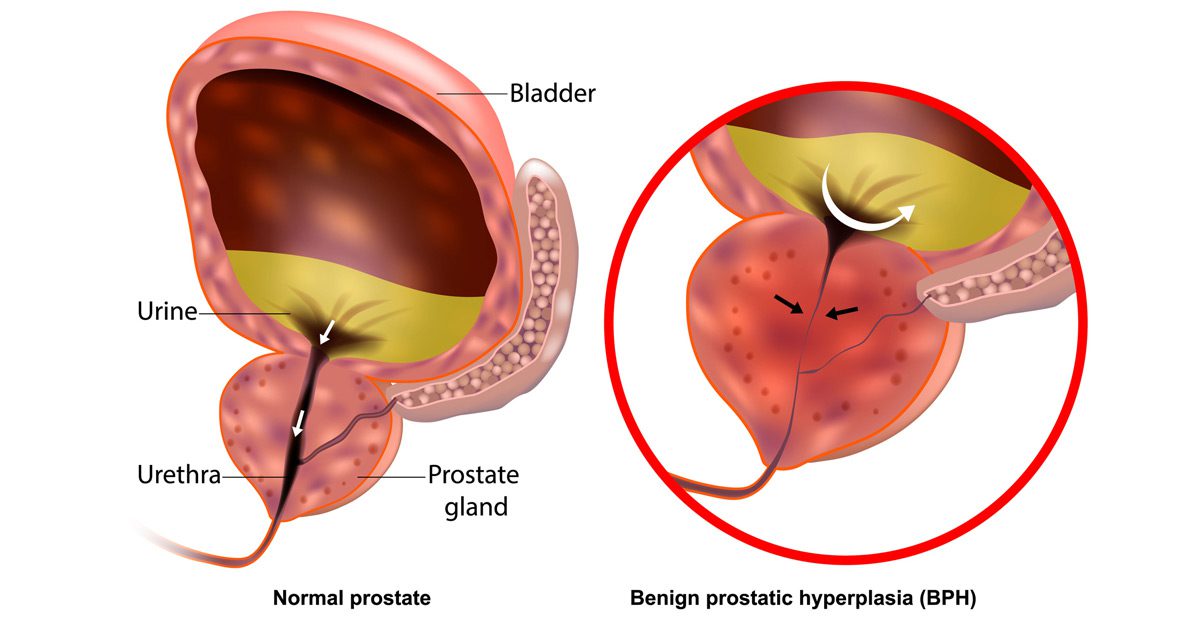
Benign Prostatic Hyperplasia (BPH), also called benign prostatic hypertrophy, is a non-cancerous enlargement of the prostate gland that commonly affects men as they age. The prostate surrounds the urethra—the tube that carries urine from the bladder out of the body. As the prostate enlarges, it can press against the urethra and interfere with normal urinary flow, leading to symptoms that affect both quality of life and urinary function.
Symptoms of BPH
Men with BPH may experience a range of urinary symptoms, which tend to worsen gradually over time. Common signs include:
- Difficulty starting urination
- A weak or interrupted urinary stream
- Frequent urination, especially at night (nocturia)
- A sensation of incomplete bladder emptying
- Urgency or the inability to delay urination
- Straining during urination
- Dribbling at the end of urination
While BPH is not cancerous and doesn’t increase the risk of prostate cancer, its symptoms can significantly affect comfort and daily life.
Causes of Benign Prostatic Hyperplasia
The exact cause of BPH is not fully understood, but it is closely linked to hormonal changes associated with aging. As men grow older, levels of testosterone decrease while estrogen levels may remain the same or increase. This hormonal imbalance is believed to contribute to prostate growth. In addition, dihydrotestosterone (DHT), a testosterone-derived hormone, may accumulate in the prostate and encourage cell growth.
Risk factors include:
- Age over 50
- Family history of BPH
- Obesity and metabolic syndrome
- Sedentary lifestyle
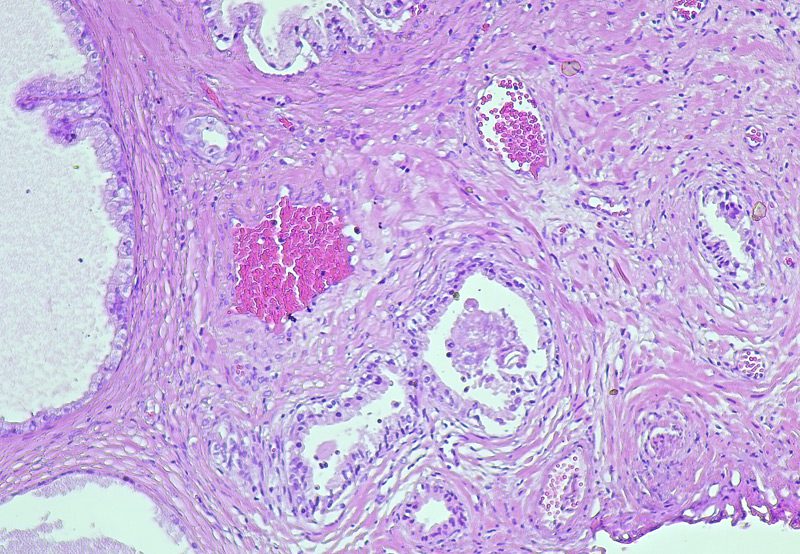
Diagnosis
A urologist may use a combination of tools to diagnose BPH, including:
- Digital Rectal Exam (DRE): To assess prostate size and shape
- Urinalysis: To rule out infection or other issues
- Prostate-Specific Antigen (PSA) Test: To evaluate prostate health
- Ultrasound or cystoscopy: To visualize the prostate and urinary tract
- Uroflowmetry and post-void residual volume testing: To measure urine flow and bladder function
Treatment Options
- Lifestyle Modifications: Reducing fluid intake before bed, limiting caffeine and alcohol, and scheduled voiding
- Medications: Alpha-blockers (like tamsulosin) to relax prostate muscles or 5-alpha reductase inhibitors (like finasteride) to shrink the gland
- Minimally Invasive Therapies: Procedures like UroLift®, Rezūm™ water vapor therapy, or transurethral microwave therapy (TUMT)
- Surgical Intervention: Transurethral resection of the prostate (TURP), laser therapy, or prostatectomy in severe cases
Next Steps
If you’re experiencing urinary symptoms consistent with BPH, it’s important to seek evaluation from a urologist. Early diagnosis and treatment can significantly improve quality of life and prevent complications such as bladder damage or urinary tract infections. A personalized care plan can help manage symptoms and maintain urinary health.
