Laser endoureterotomy is a minimally invasive procedure used to treat ureteral strictures—narrowed segments in the ureter that obstruct the normal flow of urine from the kidney to the bladder. These strictures may develop due to previous surgeries, infections, kidney stones, radiation, or congenital abnormalities. When left untreated, they can lead to pain, recurrent urinary tract infections, hydronephrosis (kidney swelling), and progressive loss of kidney function.
Symptoms of Ureteral Strictures
- Flank or abdominal pain
- Recurrent urinary tract infections
- Difficulty or pain during urination
- Blood in the urine (hematuria)
- Reduced kidney function or signs of obstruction on imaging
Causes of Ureteral Strictures
- Surgical trauma: Prior ureteroscopy, transplant, or pelvic surgery
- Stone disease: Inflammation or scarring after stone removal
- Radiation therapy: Pelvic or abdominal radiation
- Congenital narrowing: Present from birth
- Infections: Chronic infections such as tuberculosis or schistosomiasis
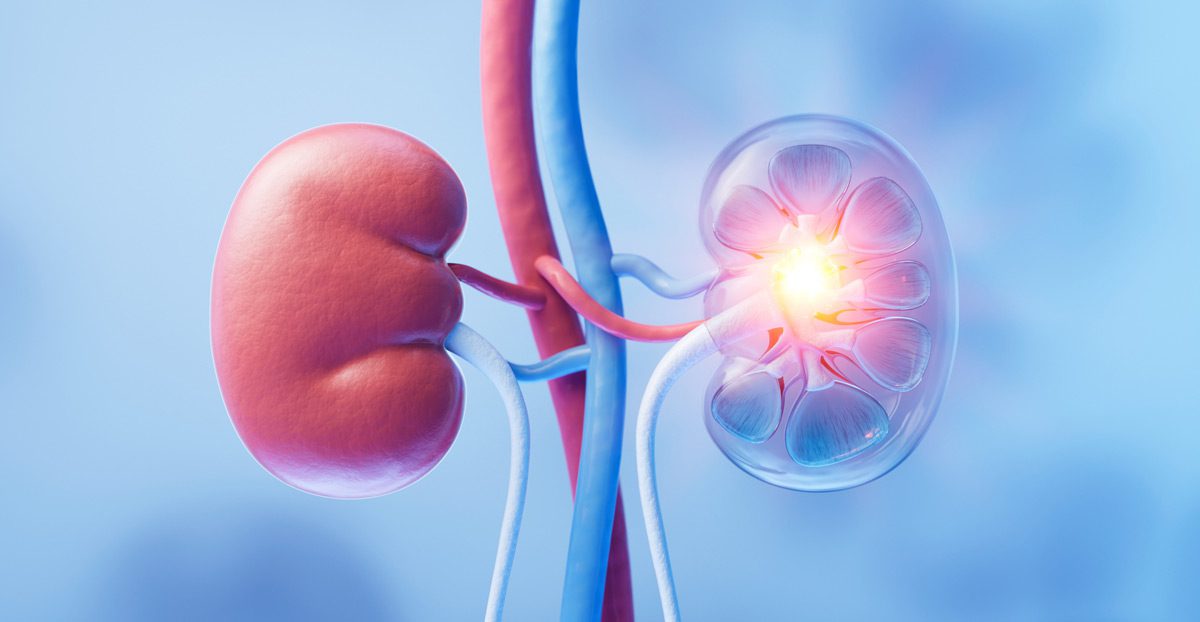
Diagnosis
Before laser endoureterotomy is performed, a thorough diagnostic evaluation is necessary to assess the location, length, and cause of the stricture. Diagnostic tests may include:
- CT urogram or MRI: To visualize the ureter and surrounding anatomy
- Retrograde pyelogram: Contrast imaging to assess the ureteral lumen
- Nuclear renal scan: To evaluate kidney function and drainage
- Cystoscopy and ureteroscopy: For direct visualization of the stricture
The Laser Endoureterotomy Procedure
The procedure is performed under general anesthesia using a ureteroscope inserted through the urethra and bladder to access the ureter. Once the stricture is identified, a precise incision is made using a Holmium:YAG laser to open the narrowed segment.
- Balloon dilation may follow the laser incision to further widen the segment.
- A temporary ureteral stent is placed to keep the ureter open during healing, usually for 4–6 weeks.
This endoscopic approach avoids the need for large incisions and is often performed as an outpatient procedure or with a short hospital stay.
Recovery and Success Rates
Recovery is generally quick, with most patients resuming normal activities within a few days. Success rates are highest in patients with short strictures (under 2 cm), non-ischemic causes, and no prior failed repairs. Regular follow-up includes imaging to confirm ureteral patency and monitor kidney function.
Next Steps
Laser endoureterotomy offers an effective and less invasive option for managing select ureteral strictures. If you’ve been diagnosed with a ureteral narrowing or are experiencing symptoms of obstruction, consult a urologist to determine whether this treatment is right for you.
